IN 2006, MEDHA DEORAS-SUTLIFF had just finished a breast cancer awareness walk near her home outside Columbus, Ohio. Deoras-Sutliff, then 39, pushed her 18-month-old daughter in a stroller around a crowded exhibit area filled with tents and tables representing various breast cancer organizations.
Although she had survived two bouts with breast cancer, Deoras-Sutliff didn’t see a place for herself in the breast cancer awareness movement. The mother of four wasn’t a fan of wearing pink, a color often associated with breast cancer. She didn’t connect with the experiences of the breast cancer patients—mostly women over 60—she had encountered during her own treatments.
But a banner displayed at one of the tables reading “Young Survival” intrigued her. A woman about her own age stood behind the table. Deoras-Sutliff stopped to chat with the woman, a representative of the Young Survival Coalition (YSC), an international organization that focuses on women 40 or younger who are diagnosed with breast cancer. “To learn there was a group of other women under age 40 who had gone through similar experiences was really life-changing,” she says.
Deoras-Sutliff’s discovery led to a career pivot—from epidemiology to cancer patient advocacy. Driven initially by a desire to understand her own breast cancer experience and then to advocate for other patients with breast cancer, Deoras-Sutliff now works to support the urgent research needs of people with rare cancers.
A First Diagnosis
Deoras-Sutliff noticed a small lump in her right breast in 1992. She was 26, just married, and working for the Ohio Department of Health HIV/AIDS surveillance unit, where she gathered data on new cases of HIV/AIDS in the state.

Medha Deoras-Sutliff is an epidemiologist and breast cancer survivor. She combines an interest in research and data with a desire to help others with cancer. Photo by Jodi Miller
She showed the lump to her doctor, who recommended a needle biopsy to collect some of the cells from the lump for examination under a microscope. “I was so young. I really went into it thinking nothing would come of this,” she recalls.
The needle biopsy showed the growth was benign. The doctor told her it was probably fibrocystic breast disease, a noncancerous condition that can cause lumps in the breasts. To be on the safe side, her doctor recommended she come back for yearly mammograms to check for changes. (While screening guidelines vary, Deoras-Sutliff would typically have been considered too young to undergo routine annual mammograms.)
Deoras-Sutliff’s father, a pathologist, explained that needle biopsies can sometimes miss cancer. “‘Why do you want to have that hanging over your head?’ he asked me.” So six months later, in early 1993, Deoras-Sutliff decided to have a quadrantectomy, an operation to remove the part of the breast containing the lump with some healthy tissue surrounding it while preserving the rest of her breast. The pathology report came back with a diagnosis of ductal carcinoma in situ (DCIS).
DCIS is sometimes referred to as stage 0 breast cancer. That’s because the cancerous cells, which start in the milk ducts, have not spread beyond the ducts to the surrounding breast tissue. The American Cancer Society estimates that about 20% of new breast cancer diagnoses are DCIS.
Deoras-Sutliff’s quadrantectomy was considered curative. “I really felt that what happened to me at 26 was just an anomaly. I went for yearly mammograms and moved on,” she says.
Facing Breast Cancer a Second Time
Over the next 12 years, “a lot of life and living happened,” says Deoras-Sutliff. She continued her work in public health until 1999, when she quit her job to be a stay-at-home mom. In 2005, she was breastfeeding her fourth child when she noticed a slight change in the area of her surgical scar. It felt like a hardened lump. “I thought at first it was a clogged milk duct,” she says, but at her next postpartum checkup, she told the OB-GYN.
An ultrasound showed a suspicious mass in her breast. This time, the biopsy suggested stage I breast cancer—a tumor 1 centimeter in size that had not yet spread beyond the breast to nearby lymph nodes. Deoras-Sutliff opted for a mastectomy and had her right breast removed. The mastectomy confirmed a diagnosis of stage I estrogen receptor-positive breast cancer.
Her oncologist recommended a short course of chemotherapy, but Deoras-Sutliff agonized over the decision. “I was looking at data that was telling me that at my early stage—with a mastectomy, clear margins and no lymph node involvement—I should not need chemotherapy,” she says. But she also was younger than 40 and on her second round of breast cancer. Today, people with early-stage breast cancer would likely have a tumor sample analyzed to predict the risk of recurrence and whether chemotherapy after surgery might be beneficial, says Nikhil Wagle, a medical oncologist at the Dana-Farber Cancer Institute in Boston. (Wagle did not treat Deoras-Sutliff’s cancer.)
Deoras-Sutliff sought second opinions from several doctors. Most of the oncologists recommended chemotherapy to kill off any errant cancer cells that may have escaped the surgery. “This was the first time I really thought about how cancer metastasizes or spreads—and how it kills,” she says.
Deoras-Sutliff completed four treatments with AC chemotherapy—a combination of two drugs used to treat breast cancer called Adriamycin (doxorubicin) and Cytoxan (cyclophosphamide). From diagnosis to final breast reconstructive surgery took eight months. “During that time, I was solely focused on myself and my immediate family—getting through it and getting well,” she says.
Drawn to Advocacy
By the time she encountered the YSC booth at the breast cancer event in 2006, Deoras-Sutliff was ready to shift her focus to something new. She began volunteering with YSC and helped to start a central Ohio YSC affiliate based in Columbus. That opportunity connected Deoras-Sutliff not only to a national breast cancer organization, but to a host of other breast cancer resources for young adults that helped her take a magnifying glass to the disease that had struck twice.
“I started to understand that breast cancer is not one disease,” she says. “Knowing what type of breast cancer you have, your genetic risk factors [and] the genomic makeup of your cancer can directly impact treatment options and access to clinical trials.” While genetic testing didn’t yield any additional pieces of information for Deoras-Sutliff—she has no known high-risk mutations, such as those found in the BRCA1 or BRCA2 genes—she saw that it did inform treatment decisions made by many of the other young survivors she worked with.
Deoras-Sutliff learned more about breast cancer by participating in Project LEAD, a week of intensive training focused on the science of breast cancer. The program, organized through the National Breast Cancer Coalition, stoked a “fire in the belly,” says Deoras-Sutliff. It combined her professional interest in scientific research with a desire to “connect with something a little bigger than just me.” She realized that if she was going to advocate on behalf of others and speak about the breast cancer experience, she needed to understand what others were going through and how research affected all people with breast cancer, not just women like her.
“I think Medha’s driving force is a passion for helping others. She’s incredibly kindhearted and generous,” says Michelle Esser, a friend whom she met at Project LEAD. “But what really excites her is data. She’s an epidemiologist by training. She wants to make sure that breast cancer advocacy decisions are based on data and evidence.”
A New Career
In 2012, the Columbus YSC affiliate Deoras-Sutliff had helped build was a flourishing support network for young women diagnosed with breast cancer in central Ohio. She began working full time as a regional coordinator for YSC, building community engagement across the Midwest and Northeast. Yet she continued to feel pulled toward projects involving breast cancer research and data.
To answer this call, in 2017 Deoras-Sutliff began working for a national nonprofit called Facing Our Risk of Cancer Empowered (FORCE), where she coordinated a program to help nonexperts cut through breast cancer research hype in the news. Next, Deoras-Sutliff became director of scientific affairs for the National Breast Cancer Coalition in 2018. There, she got a behind-the-scenes look at how breast cancer research was funded.
By this point, it had been more than 25 years since Deoras-Sutliff’s first breast cancer diagnosis. She continued going for her yearly mammogram. Each year her scans were clean. Yet, “each year I would think this is the year they’re going to find something,” she says. Deoras-Sutliff voices a fear shared by many breast cancer survivors—that the cancer will come back one day and spread to another part of the body where it can’t be stopped.
When Deoras-Sutliff looked back over the past few decades of breast cancer research, she thought, “we didn’t seem to be stopping women from dying from metastatic breast cancer, despite the millions and millions of dollars that have been invested in breast cancer research.”
Wagle, the Dana-Farber Cancer Institute medical oncologist, agrees. “We’ve made great progress with new therapies and people living longer than ever with breast cancer, but we still don’t have a cure for metastatic breast cancer,” he says.
Deoras-Sutliff met Wagle, who is a breast cancer researcher, during her years at YSC. Wagle directs the nonprofit Count Me In, which aims to engage and empower people with all cancer types, including rare cancers, by helping them more easily share their medical information, personal experiences and tumor samples with biomedical researchers for genetic analysis. “The idea is that by pooling resources, we can make faster progress toward a cure,” he says.
Deoras-Sutliff credits attendance at a Scientist↔Survivor patient advocacy program sponsored by the American Association for Cancer Research (AACR) with raising her awareness of cancer research and patient advocacy for all cancer types. (The AACR publishes Cancer Today.) The Scientist↔Survivor Program connects patient advocates with cancer scientists.
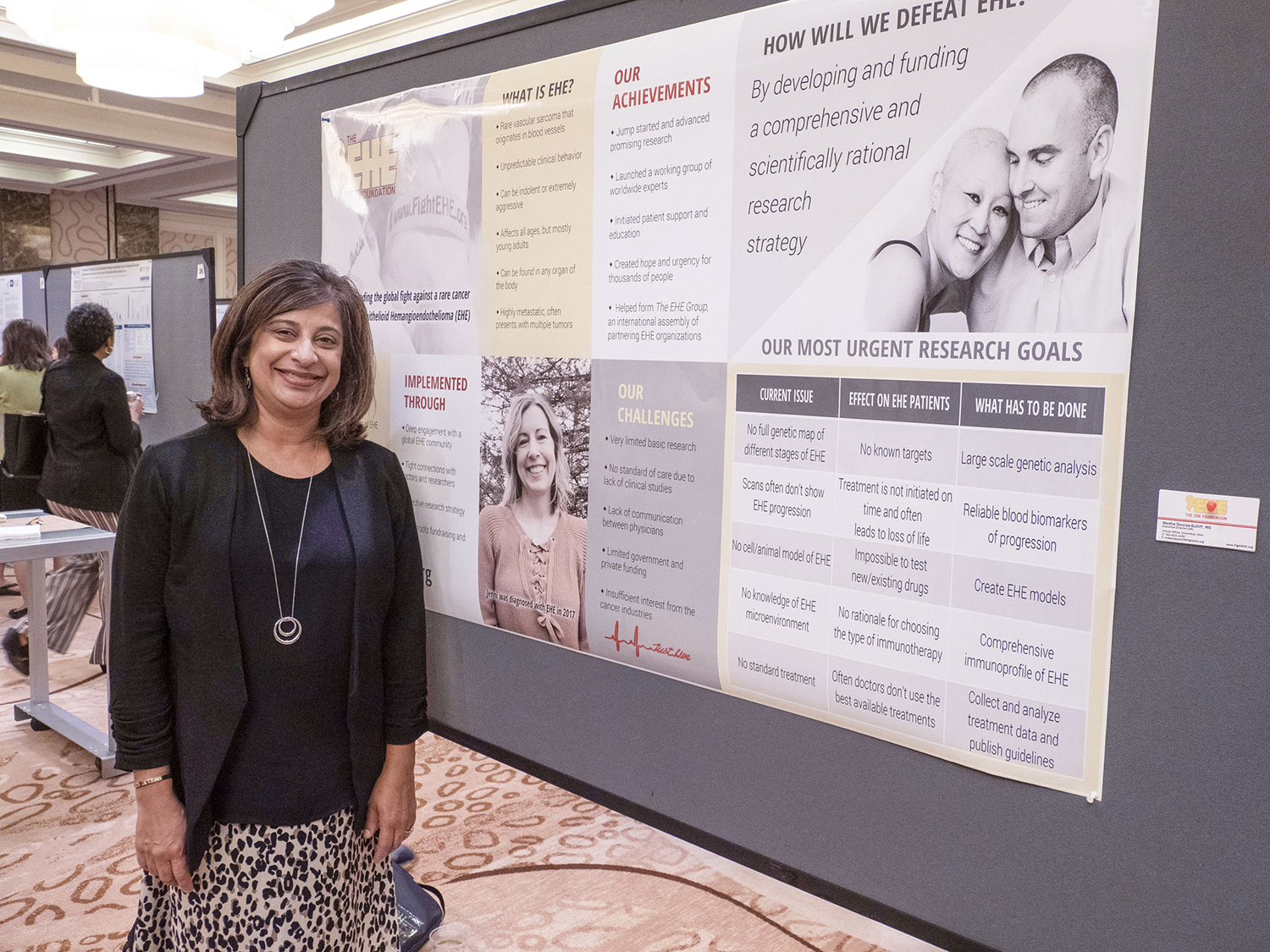
Medha Deoras-Sutliff stands before her poster describing the EHE Foundation, a patient advocacy organization she leads. Deoras-Sutliff presented the poster at a conference on cancer health disparities held by the American Association for Cancer Research in 2019. Photo © AACR / Todd Buchanan 2019
She became particularly fascinated by rare cancers, which get much less attention and research funding than breast cancer, and she was taken with the idea expressed by advocates for rare cancer patients that research on these cancers might unlock discoveries that could help people with all cancer types. An example, Wagle says, was the discovery that the BRCA2 gene was involved in Fanconi anemia, a rare bone marrow disease. BRCA2 mutations predict a higher susceptibility to breast, ovarian and prostate cancers, so research on this rare bone marrow disorder helped shed light on common cancers. Deoras-Sutliff began to think maybe answers to questions about metastatic breast cancer could be uncovered by researching rare cancers.
Hope for a Rare Cancer
Inspired by her newfound interest, Deoras-Sutliff left her career in breast cancer advocacy to advocate for patients with rare cancers. In 2019, she became the executive director of the EHE Foundation, a nonprofit organization aimed at pursuing new treatments for epithelioid hemangioendothelioma (EHE), a rare type of blood vessel tumor.
Epithelioid hemangioendothelioma is a rare cancer of the cells that line the insides of blood vessels.
EHE, or epithelioid hemangioendothelioma, is a form of cancer that starts in the cells that line the insides of blood vessels. While it can occur anywhere in the body, the most common sites for EHE are the liver, lungs and bones. The National Cancer Institute estimates that one in a million people worldwide is diagnosed with EHE. Since the disease is so rare, there is no standard treatment, though conventional therapies such as chemotherapy, surgery and radiation can be used based on where the tumor is formed. The EHE Foundation and others are working on research that could provide doctors of EHE patients with options for evidence-based treatments.
EHE felt like a natural fit for Deoras-Sutliff. She saw a lot of parallels between her breast cancer experience and the issues faced by rare cancer patients. Although breast cancer itself is common—one in eight women in the U.S. will develop breast cancer in their lifetime—Deoras-Sutliff’s young age at diagnosis and ethnicity (she was born in India) put her in a smaller breast cancer demographic. Less than 4% of all new breast cancer diagnoses occur in women under 40, and breast cancer is less common among Asian Americans than whites or Blacks.
EHE is most commonly diagnosed in adults between the ages of 30 and 50, although it can arise at any age. More women than men are affected. “I felt that I could really relate to that 28-year-old with a baby or that 28-year-old who wants to talk about fertility preservation before treatment,” says Deoras-Sutliff.
Under her direction, the EHE Foundation has partnered with the Rare Cancer Dependency Map Initiative, a program of the Broad Institute of MIT and Harvard in Cambridge, Massachusetts, to develop an EHE cell line. Cell lines help researchers study cancer behavior and responses to various therapies. She’s hoping that one day soon, research on rare cancers such as EHE might provide clues about how all cancers can be stopped from spreading in the body. “I’d like to help make that contribution,” she says.
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.





