IT WAS FEBRUARY 2019, and Alexis Browning’s leg had gone from a curiosity to a concern. For years prior, the otherwise healthy 24-year-old noticed that her right thigh seemed to be larger than her left. To her it was obvious—she’d always see it in photos. But the difference was slight enough that she had to point it out to friends and family.
“I feel like I was always showing other people, and they would react like, ‘Oh yeah, I can see it,’” Browning says.
But then she started feeling pricks of pain emanating from her thigh. That finally got her into a doctor’s office for an X-ray. The doctor told her everything looked fine, but the X-ray showed Browning’s right thigh was indeed larger than her left. Curious, the doctor ordered an MRI for a closer look.
That’s when Browning’s world started to unravel.
“They called me right away and said there was a mass spanning 18 centimeters [7 inches],” Browning recalls.
Doctors took a sample of the growth for a biopsy and ordered a full-body positron emission tomography (PET) scan. The results were harrowing. Not only was the mass cancerous, but there were also tumors in Browning’s lungs. On March 13, 2019, a day seared into Browning’s memory, the diagnosis came in: stage IV alveolar soft part sarcoma (ASPS). The doctors told Browning she’d probably had the rare cancer, which originates in soft tissues such as fat and muscles, for a decade.

Photo courtesy of Alexis Browning
Browning dove into research. She learned there are only about 80 cases of ASPS diagnosed in the U.S. each year, according to the National Cancer Institute (NCI), with treatment options scant and the prognosis poor. In patients where ASPS has spread beyond an original tumor site, five-year survival rates are between 10% and 40%, depending on whether surgery is performed. Eventually, a doctor told Browning she had between 10 and 20 years to live.
“I just remember being gobsmacked,” Browning says. “I felt like I was in the prime of my life, but my parents were absolutely terrified. Being around them made me realize the true severity of the situation.”
An ‘Oddball’ Sarcoma
Amit Sabnis, a pediatric oncologist and researcher at the University of California, San Francisco, says that sarcomas in general are rare and complicated cancers to treat. But even within that subset, ASPS is an “oddball,” Sabnis says.
Alexis Browning spoke to the American Association for Cancer Research (AACR) about her experience with alveolar soft part sarcoma for the AACR Cancer Progress Report 2023. (The AACR also publishes Cancer Today.) Read her story.
First, the demographics of patients are unusual. ASPS tends to strike during childhood. It typically starts as a small, localized tumor and grows slowly enough that it often isn’t diagnosed until symptoms develop in young adulthood. By then the cancer may have already spread to other parts of the body, as was the case for Browning.
Then comes the most troubling part: Little can be done clinically to treat it. If an ASPS tumor is caught early enough, the first line of treatment is to surgically remove it and hope for clear margins. But relapses can occur years later and tend to resurface in the brain, Sabnis says.
Chemotherapy is mostly ineffective. A drug called Sutent (sunitinib) had shown some promise in halting tumor growth, but the effects were underwhelming, Sabnis says. Another major challenge is that ASPS is so rare that it can be difficult to set up clinical trials to test potential treatments, especially since it so often appears in children, who medical guidelines typically discourage from being included in early clinical trials.
“There hasn’t been any sort of prolonged, curative therapy that we’ve been able to offer,” Sabnis says.
After her diagnosis in 2019, Browning discovered these realities firsthand. An oncologist near her hometown of Louisville, Kentucky, ordered a chemotherapy regimen for Browning. At one point, the chemotherapy pills were ready for pickup at her local pharmacy.
But Browning had also sought a second opinion, leading her to a specialist at the Dana-Farber Cancer Institute in Boston who was familiar with ASPS. The oncologist delivered a “wake-up call” on Browning’s prognosis and treatment plan, explaining that traditional treatment options like chemotherapy were unlikely to be successful. Instead, Browning received a recommendation to join a clinical trial at the National Institutes of Health in Bethesda, Maryland.
“It wasn’t a huge decision to get on the trial,” Browning says. “We didn’t feel like there were a lot of other options.”
A Flicker of Hope
Alice Chen, an oncologist who serves as head of the National Cancer Institute’s (NCI) Early Clinical Trials Development Program and its Developmental Therapeutics Clinic, is well-acquainted with ASPS. Chen specializes in both rare cancers and early drug development. She’d already led two clinical trials on ASPS when Alexis Browning walked in her door.
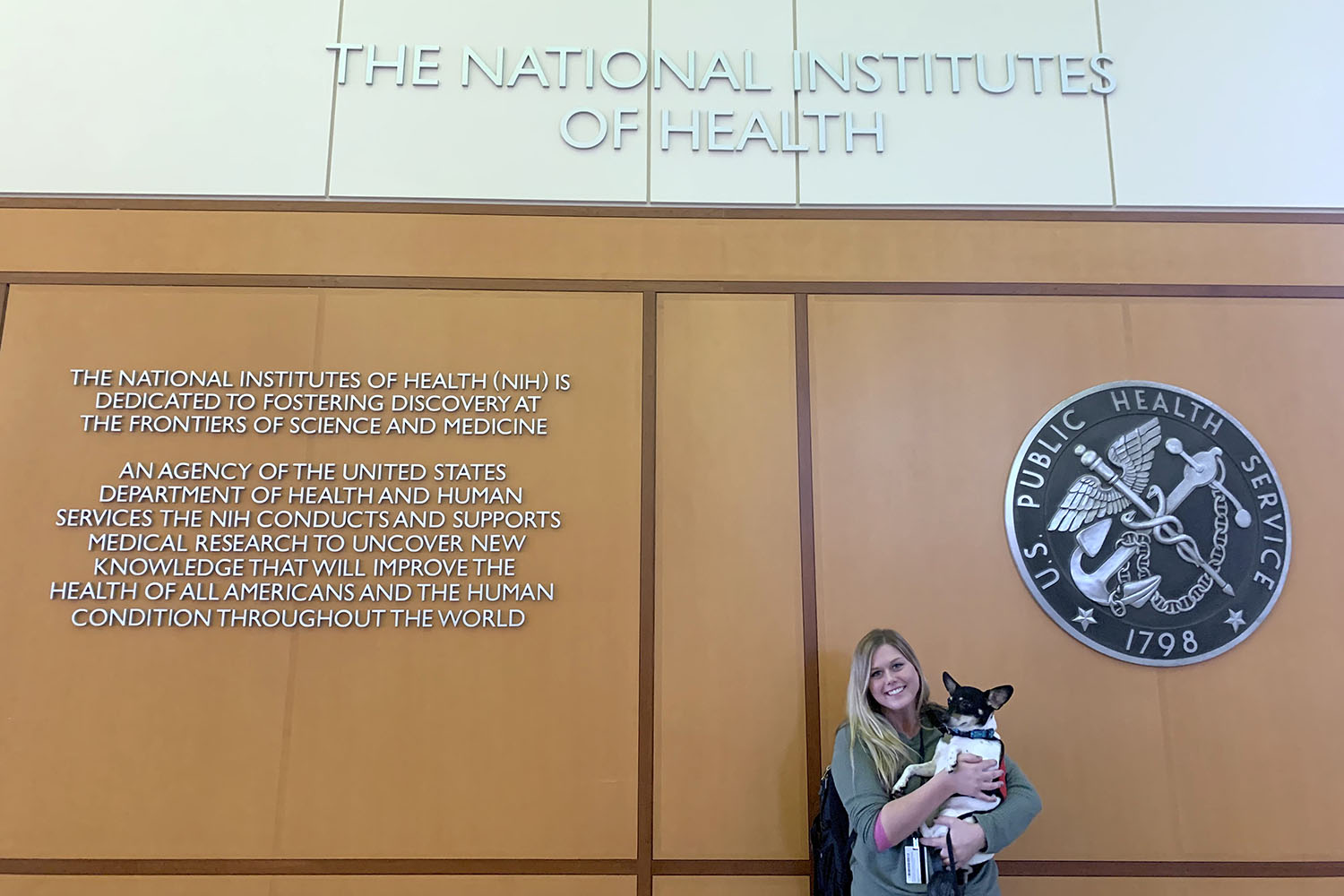
Alexis Browning received immunotherapy for ASPS through a clinical trial at the National Institutes of Health. Photo courtesy of Alexis Browning
Chen was onto something new. Researchers and clinicians were excited about Food and Drug Administration (FDA) approval of several immune checkpoint inhibitors to treat certain cancers. A colleague at the NCI’s Cancer Therapy Evaluation Program told Chen about a compassionate-use case in which a young child had been given the checkpoint inhibitor Tecentriq (atezolizumab) and seen a positive response in their ASPS. Intrigued, Chen scoured medical literature and found some cases of ASPS patients in general sarcoma trials whose cancers responded to Tecentriq, encouraging a closer look at this treatment.
Starting in late 2017, Chen launched a clinical trial that gave Tecentriq to 52 patients with ASPS who were ineligible for surgery and followed them for two years. Of those, 18 saw their tumors shrink by 30% or more and one was in complete remission. The results led to FDA approval of Tecentriq for ASPS in December 2022. Even better, Chen says, the drug is viewed as highly tolerable with few major side effects.
“I was very thrilled,” Chen says. “We’ve had marriages. We’ve had high school, college graduations [for some patients]. It was very gratifying to see that people are making plans and living their lives … allowing patients to really continue to do what they normally would do.”
Browning didn’t see her tumors shrink during the trial, but says the drug appeared to halt their growth. At first, she flew from Louisville to Washington, D.C., every three weeks to receive Tecentriq intravenously. Eventually, she was able to switch her treatment to a cancer center about three hours away in Ohio. After FDA approval in 2022, she could receive it right in her hometown of Louisville.
But with the tumor in her leg causing pain and limiting her lifestyle, Browning made a difficult decision to leave the trial in May 2021 and have surgery on the primary tumor. It was a gamble, but Browning’s surgeon told her he obtained clean margins after removing the tumor. There has been no sign that the operation exacerbated the spread of the disease, and she continues to receive Tecentriq.
Still, there are struggles. Due to her illness and treatment, pregnancy is not an option for Browning. She had her eggs frozen, but she has complicated feelings around surrogacy. And because she is not technically in remission, with tumors still present in her lungs, she’s ineligible to adopt a child.
While Tecentriq and surgery have restored much of Browning’s quality of life, the inability to become a mother still leaves her feeling “cheated.” She also knows the long-term effectiveness of Tecentriq is uncertain, and that the drug didn’t work as well for other people in the trial.
For all of these reasons, she advocates and hopes for more groundbreaking developments.
“Wouldn’t it be amazing to actually see light at the end of the tunnel?” Browning asks.
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.





