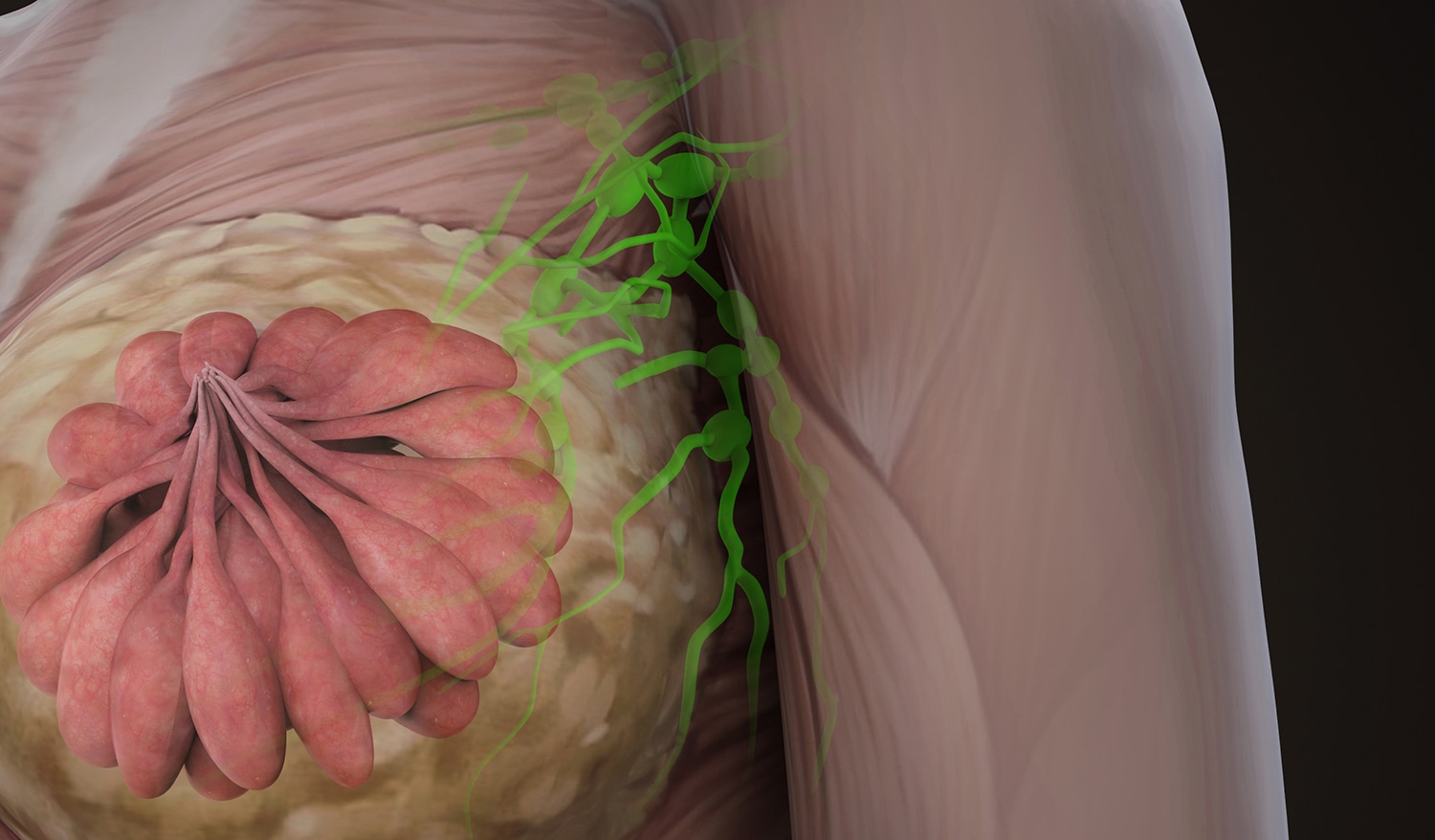
When a patient is diagnosed with invasive breast cancer, surgeons remove lymph nodes from the armpit to see if the cancer has spread. In the past, this meant removing many lymph nodes from throughout the armpit. In recent decades, some breast cancer patients have been able to undergo sentinel lymph node biopsy, in which surgeons remove just one lymph node or a few lymph nodes where the cancer is most likely to have spread.
It’s been less clear which patients diagnosed with ductal carcinoma in situ (DCIS)—a noninvasive precancer of the milk ducts—need to have their lymph nodes tested for cancer. A study published in the December 2019 issue of JNCI Cancer Spectrum finds that older patients with DCIS who undergo breast-conserving surgery, also known as lumpectomy, have similar breast cancer-related outcomes regardless of whether they receive sentinel lymph node biopsy.
“Our study actually showed that there is no benefit of sentinel node biopsy in terms of breast cancer mortality, breast cancer recurrence or invasive breast cancer,” at least in older patients, says study co-author Shi-Yi Wang, a health services researcher at Yale School of Public Health in New Haven, Connecticut.
The researchers used the Surveillance, Epidemiology, and End Results-Medicare database to identify women ages 67 and older who were diagnosed with DCIS from 2001 through 2013 and received breast-conserving surgery. The researchers matched the 1,992 women who received sentinel lymph node biopsy with 3,965 women in the database who did not have the procedure, making sure the two groups were similar based on factors like age, geographic location and tumor characteristics.
First, the researchers looked at whether the women had a recurrence of their DCIS and went on to need a mastectomy. There was no significant difference between the two groups. Both groups also had a similar rate of invasive breast cancers later appearing in the same breast as their DCIS. Finally, women who received sentinel lymph node biopsy had a similar rate of death from breast cancer as those who did not undergo the lymph node procedure. The researchers tracked these outcomes through 2013 and 2014.
The rate of any type of lymph node biopsy in patients with DCIS who received breast-conserving surgery increased from around 20% to 44% between 1998 and 2011 due to a rise in sentinel lymph node biopsies. The rate of sentinel lymph node biopsy in this group increased from around 7% to 39%, while the rate of more extensive lymph node dissection fell from 13% to 5%.
“A sentinel node biopsy is not an entirely benign procedure,” says Deanna Attai, a breast surgeon at UCLA Health in Los Angeles who was not involved in the research. The procedure can cause bleeding, pain or bruising at the biopsy site, infection, allergy to the dye used to map the lymph nodes or painful swelling of the arm, called lymphedema, from damage to the lymph nodes. Patients undergoing a sentinel node biopsy can have a 6% to 10% risk of lymphedema. “They can develop it after removing even one lymph node. This side effect can be lifelong,” Attai says.
Harold Burstein, a medical oncologist at Dana-Farber Cancer Institute and Brigham and Women’s Hospital in Boston, says DCIS is a “preinvasive cancer problem we want to treat to prevent the development of breast cancer, like we remove colon polyps so they don’t become colon cancer.” For women with DCIS who undergo breast-conserving surgery, Burstein notes that “it’s a well-accepted guideline that there is no need to do a sentinel node mapping procedure.” If a surgeon finds an unexpected, invasive cancer during a lumpectomy, they can always do a subsequent sentinel lymph node biopsy.
American Society of Clinical Oncology and National Comprehensive Cancer Network (NCCN) guidelines recommend sentinel lymph node biopsy for DCIS only in extenuating circumstances, says Benjamin Anderson, a breast cancer surgeon at the University of Washington and Fred Hutchinson Cancer Research Center in Seattle and vice chair of the NCCN Breast Cancer Panel, the group that comes up with guidelines for treating breast cancer.
“The value of a sentinel node biopsy for pure DCIS is quite limited,” he says. One indication for a sentinel lymph node biopsy is if a patient is at high risk for invasive cancer based on the size and extent of abnormal cells in their milk ducts. Another indication is when a woman is undergoing a mastectomy as part of treatment, since it is the last chance to perform sentinel lymph node biopsy. The breast has to be present to find the sentinel lymph nodes. If the patient receives a mastectomy and does not receive a sentinel lymph node biopsy, she may later need to undergo more extensive lymph node removal should lymph node surgery prove necessary.
“Wang is providing us with evidence that we can step further away from doing a sentinel node biopsy, in older patients in particular, where the likelihood of the benefit of sentinel node biopsy is less,” says Anderson.
Although the new study applies to older women, Anderson says younger women with cancer should also ask their surgeon if a sentinel node biopsy is necessary and should only undergo one if “there is something exceptional about their case.”
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.