Sue Friedman never knew her father’s mother, who died of some type of abdominal cancer long before she was born. Yet there’s a good chance that her own diagnosis of stage II breast cancer at age 34 was the result of a genetic mutation that was lurking in that branch of her family tree.
In 1997, shortly before she was diagnosed with invasive cancer, the veterinarian from Coral Springs, Fla., read a magazine article in a doctor’s office about a simple blood test that could identify inherited mutations in the BRCA1 and BRCA2 genes. People with these mutations face increased risk of developing breast and ovarian cancer. Friedman learned that women of Ashkenazi (Eastern European) Jewish descent, like herself, are more likely to carry BRCA mutations, and she quickly realized how little she knew about her young grandmother’s illness.
After her own diagnosis, Friedman sought genetic counseling and then a blood test for the mutations. In February 1998, she received the news: She had a BRCA2 mutation. Friedman began to suspect that her paternal grandmother may have had ovarian cancer. “My dad talked about his mother all the time,” says Friedman, who in 1999 founded Facing Our Risk of Cancer Empowered (FORCE), a nonprofit organization that focuses on getting the word out about hereditary breast and ovarian cancer. “But other than [his] telling me that she died young of cancer, and that the doctors couldn’t do much for her once it was discovered, her illness and death were not mentioned.”
Like Friedman, many people don’t know their family history of cancer. As recent studies have shown, a person’s knowledge of family members’ health is frequently imprecise or even flat-out wrong. But taking steps to uncover these hidden clues to cancer risk may pay off: Even when a person doesn’t have a known inherited cancer mutation, knowledge of family cancer history can inform decisions about cancer screening. A family history may also play a role in whether a patient seeks genetic testing or learns about a risk of developing additional cancers. Such information may even influence treatment choices for some patients, Friedman suggests.
The Value of an Accurate History
Only about 5 to 10 percent of all cancers are the result of inherited genetic mutations, and most cancers occur in people with little or no family history of the disease. But nearly one in four people are estimated to have a family history that suggests a predisposition to cancer, according to a study published in the journal Genetics in Medicine in November 2010.
Identifying those individuals who have a family history of a specific cancer is important, says Phuong Mai, a medical oncologist with the National Cancer Institute (NCI) who was not involved with that study, “because the presence of cancer in relatives might suggest that the individual’s risk for that same cancer is increased.”
And that’s knowledge on which many individuals may be able to act to reduce their risk. Having a family history of cancer converts basic cancer screening into cancer surveillance, explains Margaret Eberl, a family practice and preventive medicine physician in Buffalo, N.Y. Knowledge of one’s family history may change not only at what age cancer screening should begin, but also how frequently the screening occurs.
Talk to Your Family!
If you’re diagnosed with cancer, tell your family members. Share your story. Remind them to get screening and encourage them to make healthy lifestyle choices to reduce risk.
The Surgeon General, in 2004, declared Thanksgiving to be National Family History Day, an annual event during which family members can talk about their health history because they’re often already together. Ask your relatives specific questions about cancer, including information they have about relatives who are not in attendance.
People with a strong family history of colorectal cancer, for example, should undergo screening with colonoscopy every five years, beginning at 40 or 10 years less than the age of the youngest person diagnosed in the family, according to the American Cancer Society (ACS). During a colonoscopy, polyps can be found and removed, including those that may be precancerous. For individuals not at high risk, guidelines recommend colonoscopy every 10 years beginning at age 50, or use of an alternate screening method.
For breast cancer, the ACS recommends that women at high risk—including those who have a BRCA mutation or a first-degree relative with a BRCA mutation—begin to receive annual screening by mammography and MRI by age 30, which is 10 to 20 years earlier than the guidelines that cancer organizations recommend for women at average risk. Screening may detect breast cancer early; however, only limited evidence supports the age at which to begin screening, so patients are advised to discuss personal circumstances with their health care providers to determine the best course of action.
Beyond screening, says Eberl, “rapidly accumulating evidence” is showing that lifestyle interventions—such as maintaining a healthy body weight, getting more exercise, quitting smoking and limiting alcohol consumption—may contribute to lower risk of cancer for someone with a family history.
Some cancer patients with a strong family history of cancer may have an inherited cancer syndrome that can be identified through genetic testing. For patients with one of these syndromes, there may be an increased risk of developing a second cancer, either of the same type or a related one, according to Mai.
Knowing about her increased cancer risk was especially important to Friedman: Her inherited BRCA2 mutation meant that she has hereditary breast and ovarian cancer syndrome. It put her at extremely high risk of developing a second breast cancer and ovarian cancer—which often goes undetected and undiagnosed until it has advanced to a late stage. She decided to reduce her risk by having surgery to remove her noncancerous breast as well as her ovaries and uterus.
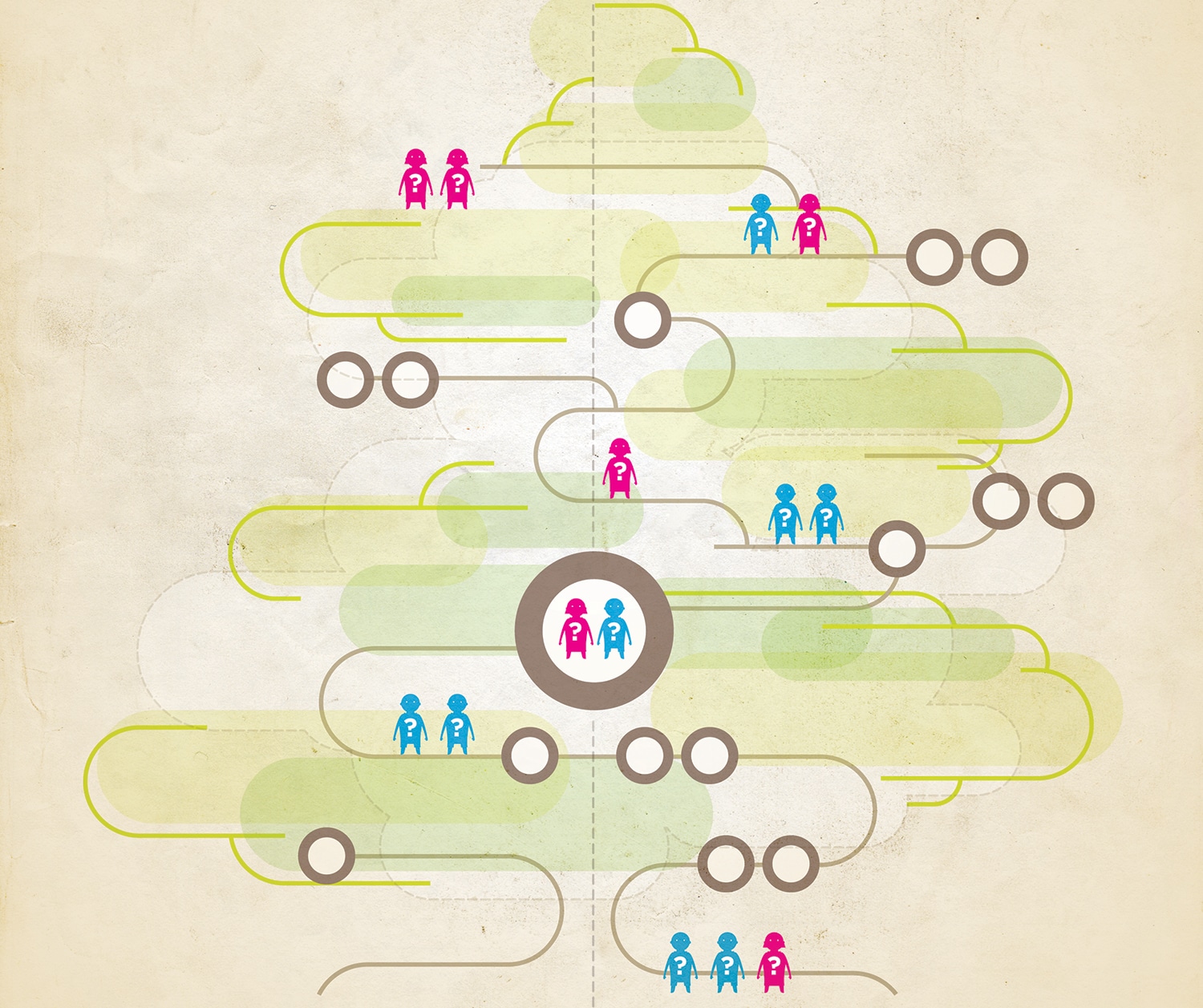
Friedman had most likely inherited her risk-raising BRCA2 mutation from her grandmother, who passed it on to her father, who then passed it on to her. So she began alerting her family members—including cousins she hadn’t spoken with in more than 20 years—about their potential risks, as well. The conversations were not easy, but Friedman believed it was her obligation to inform. “There are still many people who do not understand hereditary cancer or the risks,” she says.
Knowing Your History
The more researchers study family cancer histories, the more evident it becomes how few families are sharing complete information about potentially dangerous and inherited conditions.
Mai recently led a study of family cancer history knowledge using data from a telephone survey of Connecticut residents. Connecticut has the oldest cancer registry in the United States, with records dating to 1935. That registry—combined with other resources, such as Medicare claims, medical records, and death certificates—allowed Mai’s group to determine which of the survey participants’ relatives, living or deceased, had in fact had cancer.
The results, published in the May 18, 2011, Journal of the National Cancer Institute, showed that when respondents reported no family history of cancer in a relative they were usually correct. However, they were not as accurate at reporting a positive cancer diagnosis in their relatives. Of the people who said a first- or second-degree relative had lung cancer, just 40 percent were correct, and of those who said a first- or second-degree relative had breast cancer, only 61 percent were correct.
Keeping a Family History
Several online tools can help you compile a complete and accurate family history. Here are two places to start:
My Family Health Portrait
Created as part of the U.S. Surgeon General’s Family Health History Initiative, this site can help you collect, organize, save, print out and share your health history.
Family HealthLink
This Ohio State University Medical Center tool can help you assess your family’s health risks.
Part of the problem, Mai’s team discovered, was that a reported cancer often turned out to have been a different type, sometimes one that had metastasized from another area of the body. Respondents also frequently reported that a relative had cancer when the individual had a benign condition.
“It is important to obtain accurate information about the origin of the cancer and age of diagnosis for each relative’s cancer,” stresses Dianne M. Finkelstein, a biostatistician at Massachusetts General Hospital in Boston. “For example, one might hear that an aunt died of liver cancer, but it is possible that the aunt’s cancer began in the colon and later spread to the liver.”
A recent review of family history information collected from more than 43,000 women undergoing mammography screening at a community hospital also sheds some light on the specific gaps many families have in their cancer histories. Respondents significantly under-reported the major cancers (breast, colon, prostate, lung and ovarian) that statistically would have been expected to occur among this number of families. What’s more, women reported less cancer on their father’s side of the family than their mother’s side, and they reported less cancer among aunts, uncles and grandparents than among their immediate family members, such as their parents.
“We were surprised at the extent of under-reporting,” says Elissa M. Ozanne, the lead researcher on the study, which is scheduled for publication in August 2012 in the Journal of Genetic Counseling.
Ozanne, who is a risk assessment and decision analyst with the Institute for Health Policy Studies at the University of California, San Francisco, says that the accuracy of a family history can be improved if both the patient filling out the family history questionnaire and the health care professional asking for the information recognize common gaps. A health care provider or a patient who knows that paternal history is less accurately reported than maternal, for example, can probe further into that area. “I think it is important for people to remember to talk to all relatives and not shy away from the difficult topics,” Ozanne adds.
Mai agrees. “It can be awkward or uncomfortable to discuss cancer diagnoses with one’s relatives, but since accurate information is best obtained from the person with cancer, and since the presence of cancer in one’s close relatives may influence one’s own health care, we encourage everyone to discuss this information with their close relatives.”
Compiling a family history is not a one-time event, experts note. Individuals need to keep tabs on their family members’ diagnoses with cancer and other diseases. A study of patient data from the Cancer Genetics Network, a national population-based cancer registry in the U.S., published July 13, 2011, in the Journal of the American Medical Association (JAMA), recommends updating family history every five to 10 years with the help of a primary care physician. This is especially important between ages 30 and 50, when changes in family cancer history may justify more intensive screening, particularly for breast and colorectal cancers.
“Many patients make lists of topics to discuss with their doctor before an appointment, and we hope that they add changes in their family history to that list,” says Finkelstein, one of the lead researchers on the JAMA study. She recommends doing this each year at annual checkups. “Knowing the details of your family’s cancer history and communicating this information to your physician is the best way to determine your level of cancer risk.”
Family History and Adoption
It can be especially challenging for individuals who were adopted to compile an accurate family history. Contact the agency that facilitated your adoption and ask if any pertinent records exist. For more information, check out Livestrong’s Family Medical History for Adopted Children webpage.
The bottom line in helping improve the accuracy of a family history in your file at your doctor’s office, says Eberl: “Prepare for your visit.” And if your doctor does not ask about family history, be sure to bring it up.
Basically, a primary care physician should be informed about any first- or second-degree relatives who were diagnosed with cancer. The most beneficial information beyond the primary site of the cancer is the age of the family member at time of diagnosis. Several online tools can help in the collection of an accurate family history.
The good news down the road is that the widespread adoption of electronic medical records could make maintaining an accurate family history easier. “For now, we are just trying to capture the history of the relatives who are not with us now or who won’t be with us in the next few years,” says Ozanne. “But as we age, collecting a family history will get easier because we will have electronic mechanisms to keep track of this for us.”
Just as it does today, this information will help doctors guide patient care. Meanwhile, emphasizes Mai, individuals should keep in mind that a family history of cancer does not mean a person should live in fear of a cancer diagnosis. “It is important to remember,” says Mai, that “a ‘strong family history’ is not an automatic death sentence.”
Or, as Friedman puts it, “Genetics are not destiny.”
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.