ADDING IMMUNOTHERAPY to standard care can help reduce recurrence risk for people with locally advanced head and neck cancers, according to a study presented April 27 at the American Association for Cancer Research (AACR) Annual Meeting 2025 in Chicago. (The AACR publishes Cancer Today.)
People diagnosed with head and neck cancer typically undergo surgery to remove the tumor, followed by radiation and, in some cases, chemotherapy to reduce their risk of the cancer returning. While this has been standard care for two decades, not all patients respond to this regimen, so researchers are investigating additional therapies that could help control the disease.
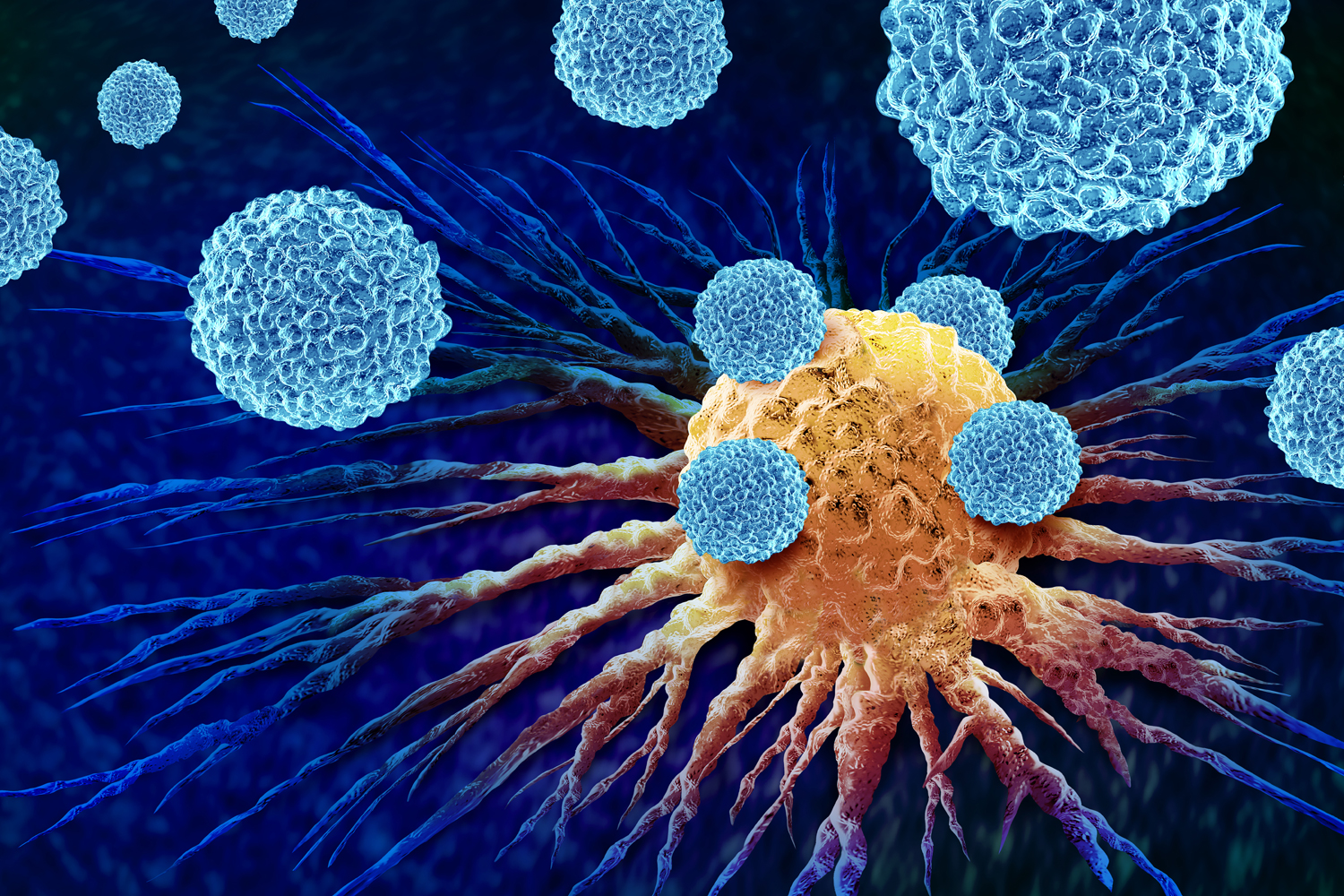
Immunotherapy, whether administered before or after surgery, is one approach that can potentially benefit people with head and neck cancer. Prior to surgery, immunotherapy can enhance the immune system’s response and help it to attack cancer cells. After the tumor is removed, immunotherapy can direct immune cells to kill any residual disease.
Researchers enrolled 714 people with stage III or IV head and neck squamous cell carcinoma in a phase III clinical trial. While all participants received standard care, 363 people were randomly assigned to also receive the immune checkpoint inhibitor Keytruda (pembrolizumab) both before and after surgery. These participants received two preoperative cycles of Keytruda and then 15 cycles after surgery. While standard care takes three months, adding immunotherapy extends the treatment time to nine months, according to Ravindra Uppaluri, the study’s lead author and director of head and neck surgical oncology at Dana-Farber Cancer Institute in Boston.
Investigators evaluated event-free survival, which is the time until a person has a recurrence or dies. After a median follow-up period of 38.3 months, participants given immunotherapy were 27% less likely to have a recurrence than those who received standard care. People who received immunotherapy had an event-free survival of 51.8 months, compared with 30.4 months for those who did not receive immunotherapy—a nearly two-year difference.
PD-L1 Status and Head and Neck Immunotherapy
The study found immunotherapy’s benefits were most pronounced in people whose tumors expressed PD-L1, a protein that blocks the immune system from attacking cancer cells. Among participants whose tumors had high PD-L1 expression, participants in the immunotherapy group had a 13.7% higher major response rate, meaning the tumor was found to have shrunk by more than 90% by the time of surgery, and a 34% lower recurrence rate than those treated with standard care.
Additionally, researchers analyzed the tissue removed during surgery. People who had standard care exhibited more high-risk features, such as more cancer cells in lymph nodes and in the edge of the excised tissue, than those who received immunotherapy. Because they had fewer high-risk features, more people who received immunotherapy did not need chemotherapy after surgery.
Both groups experienced similar rates of side effects, with around 82% of all participants having at least one treatment-related side effect. Common side effects included altered taste, dry mouth, fatigue, mouth inflammation, nausea and skin injury from radiation. Among people who received immunotherapy, 10% experienced severe or life-threatening immune-related side effects, including one death from lung inflammation.
The study’s findings should make administering Keytruda before and after surgery the new standard of care for people with resectable locally advanced head and neck cancer, according to Uppaluri. “We’ve waited for 20 years for something like this in head and neck cancer,” he said.
“This is a very exciting study and potentially practice-changing data, which seems to represent a potential new therapeutic option for these patients,” said Ryan B. Corcoran, a medical oncologist at Mass General Cancer Center in Boston, who was not involved in the study.
Beyond changing the standard of care, the results open new avenues for investigation into how to reduce the amount of treatment people with head and neck cancer must receive to control the disease, Uppaluri said. “This is very exciting because in head and neck cancer, in particular, this really sets the stage for us to think about other approaches,” he said. If patients have a complete response to immunotherapy, one possibility could be skipping surgery altogether, according to Uppaluri.
Researchers will continue to follow trial participants to determine overall survival outcomes. Uppaluri said future studies should evaluate delivering immunotherapy before surgery and after surgery separately, administering immunotherapy combinations prior to surgery, and delivering immunotherapy and combined radiation and chemotherapy at separate times.
Cancer Today magazine is free to cancer patients, survivors and caregivers who live in the U.S. Subscribe here to receive four issues per year.